Zenbox
Research / Cultural probes / Interaction design / Prototyping / Healthcare
A product designed to assist caregivers bring alternative care to their loved ones suffering with depression.
PREMERA INSURANCE, SEATTLE
About the project
- Premera, one of the prominent healthcare insurance companies in the Pacific Northwest region, provided us with a task to imagine a better means for caregivers to attain the right care, and support their care recipients.
- We were given 12 weeks to research, prototype and build a final design response.
Team & role
- Timeline and duration: September 2018 - December 2018 (12 weeks)
- I worked with Nora Owens and Samantha Baker while being mentored by Audrey Desjardins and Michael Smith.
- Deliverables: secondary and primary research, cultural probes, prototyping and testing, information architecture, user-flows, UI design, and UI spec document.
Challenge
Our problem area was to imagine a better means for caregivers to attain the right care, create a plan, and support their care recipients.
During our initial few weeks of being provided with the challenge, we performed a lot of secondary research and literature review. Moreover, all of us somehow had some interaction with depression. Consequently, we decided to dig deeper into the field and turned our focus towards mental health care.
Opportunity
We started off by understanding the problem space better. Our initial research showed the immense scale of depression in adults around the US.
16.2 million adults in the United States experience depression each year, making it the leading cause of disability.
65% of U.S. adults with depression did not receive treatment last year. And of these, less than 36% sought treatment of any kind in the first 90 days after diagnosis.
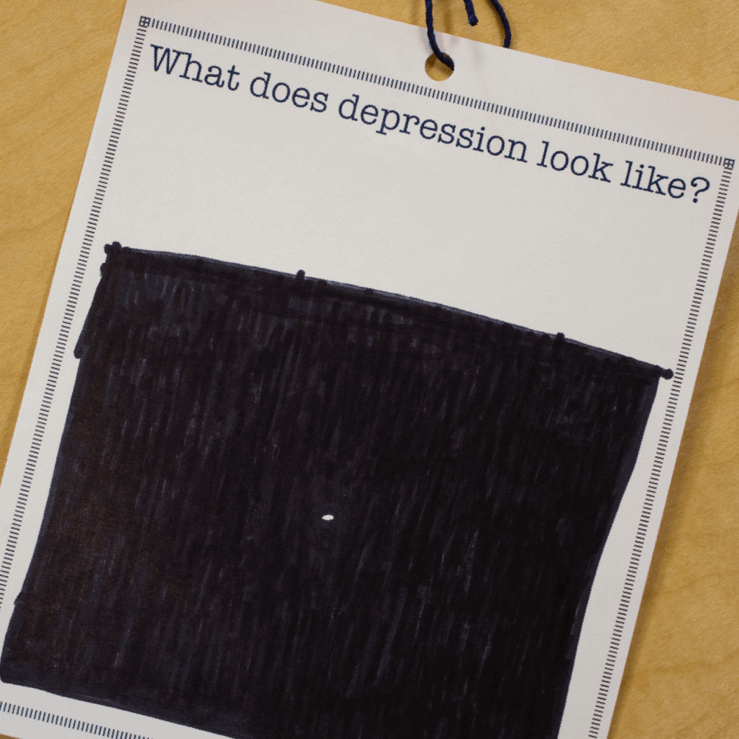
Response to a probe placed in the streets of Seattle.
Understanding the problem
We dug deeper to understand the underlying issues which prevent such a huge majority of diagnosed patients aren't receiving treatment.
-
Patients often many times doubt the diagnosis
Most patients are diagnosed by their primary care practitioner, often making an appointment for other reasons (such as fatigue, pain, or sleeplessness). Because they have yet to self-identify that they are suffering from depression, they often do not believe their doctor’s diagnosis and are hesitant to recognize their illness.
“I kept realizing [my symptoms of depression] every now and then...because [I have Bipolar II disorder], there would be periods of few days where I couldn’t sleep and then be extremely normal for a month. No one took me seriously, so I kept questioning it..”
-
Social stigma permeates all aspects of the experience
Those who feel internalized stigma are found to be less likely to engage in help-seeking behaviors. Patients often feel scared and embarrassed to talk to a doctor, causing a reluctance to seek help.
We sensed negative self-talk in responses to our “What does depression look like?” cultural probe, placed at the University of Washington.
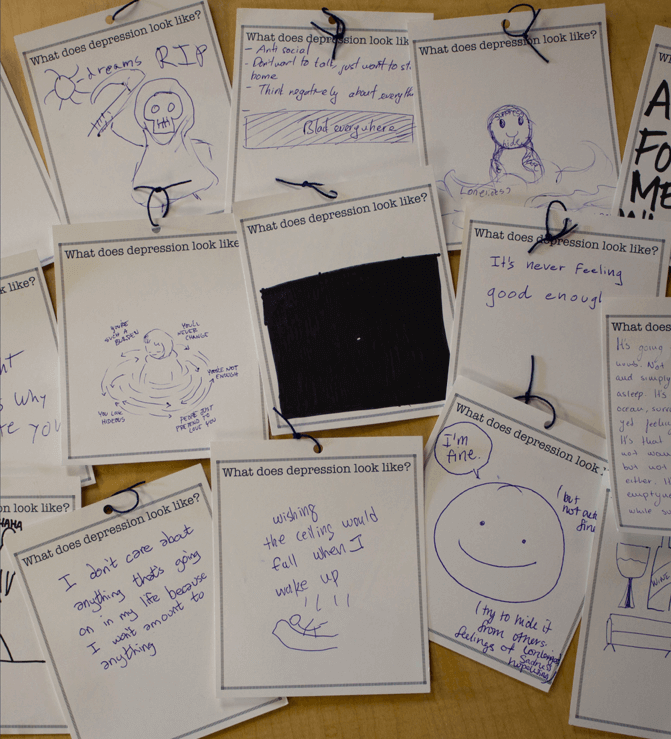
The responses we received made us surmise how different depression is recognized as in society.
-
Fear of medication keeps people from seeking treatment
Due to stigma, many people don’t like the idea of taking medications or have the perception that they’re weak if they do so. The cost of medication and the time and commitment it takes to adjust to it also acts as a barrier.
“People try the meds, start to feel ok, then get off them. It’s a never-ending cycle. With diabetes, you can go get a blood test, but mental health is very subjective.”
-
Immense issues with existing treatment options
Our research found a typical long wait to get a first appointment (2-3 weeks average) with appointments usually being only 22 minutes long. Furthermore, at the appointment, the patient needs to put the effort into articulating the complexities of their mental state and well-being.
Moreover, people are not informed of the full range of treatment options available to them.
“I was building myself up from scratch. I didn't have much to say when asked why I was there, I didn't have a specific issue to work with. She [therapist] couldn’t help me, and I looked for someone else.”
“My psychiatrist suggested me to join Yoga Therapy classes after 6 months. That helped me calm down my nerves a lot.”
But what about the caregiver?
After understanding the entire spectrum of issues around patients, we now dug deeper to see what issues do caregivers of patients with depression face.
- Caregivers of those with mental illness provide on average 32 hours of care a week, more than a typical U.S. caregiver.
- These caregivers are an integral and often the only source of unpaid help for adults with mental or emotional health issues.
Along with our probe asking “Who do you know with a mental health condition?”, we solicited stories about what it is like to support their loved one.
We found that many caregivers may be unsure of how to best provide support, and are even doubtful of what their loved ones want.
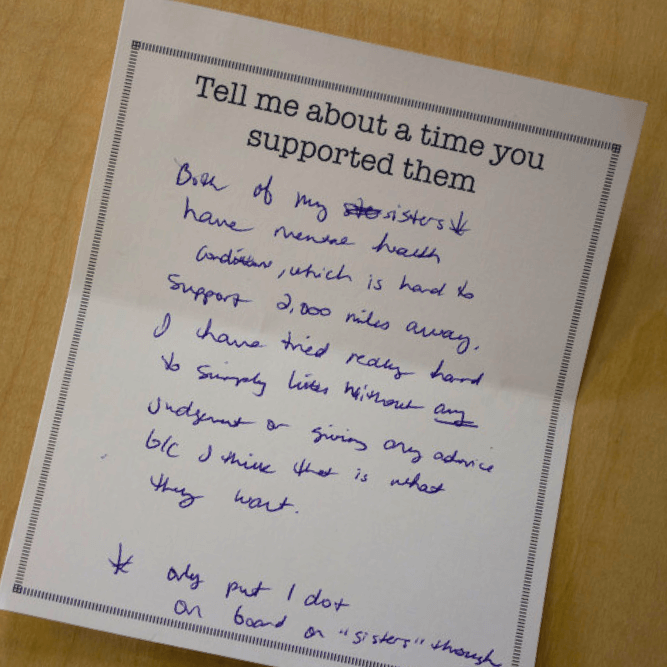
“Both of my ste sisters have mental health conditions, which is hard to support 2,000 miles away. I have tried really hard to simply listen without any judgment or giving any advice b/c I think that is what they want."
Iterated problem statement
Following our research phase we rethought our statement which gave us a better and clearer picture of what we wished to achieve with our design solution.
How might we support caregivers of adults with depression in finding the right care and supporting their care recipients?
The outcomes we hoped to achieve in our design response:
- Educate caregivers about ways they can help their care recipient.
- Provide caregivers with the tools to make an informed choice with their care recipient.
- Assist the care recipient and caregivers in overcoming existing social stigmas*.
*Stigma includes ill perceptions towards taking anti-depressants, talking about one’s depression, going to a therapist, pursuing alternative medicines, a belief in self-cure or that one can “snap out of it”, and that people with depression are weak.
Ideation
In our ideation process, we utilized many methods including 4 x 4s, 8 x 8s, polar opposites, and braiding. 90 thought-through ideas were down-selected to 20 and then to 3 final ideas.
Discussions with Premera representatives, other experts in field and various books helped us frame our criteria for down-selection.
Subsequently, we examined the strength of each with regard to the:
- Role of the caregiver
- Consideration of privacy
- Ability to get the patient directly to a care provider
- Ease of use
- Effort required by the patient
- How innovative the idea is
We negotiated combinations of our ideas to come to three proposed responses that can each comprehensively address our desired outcomes.
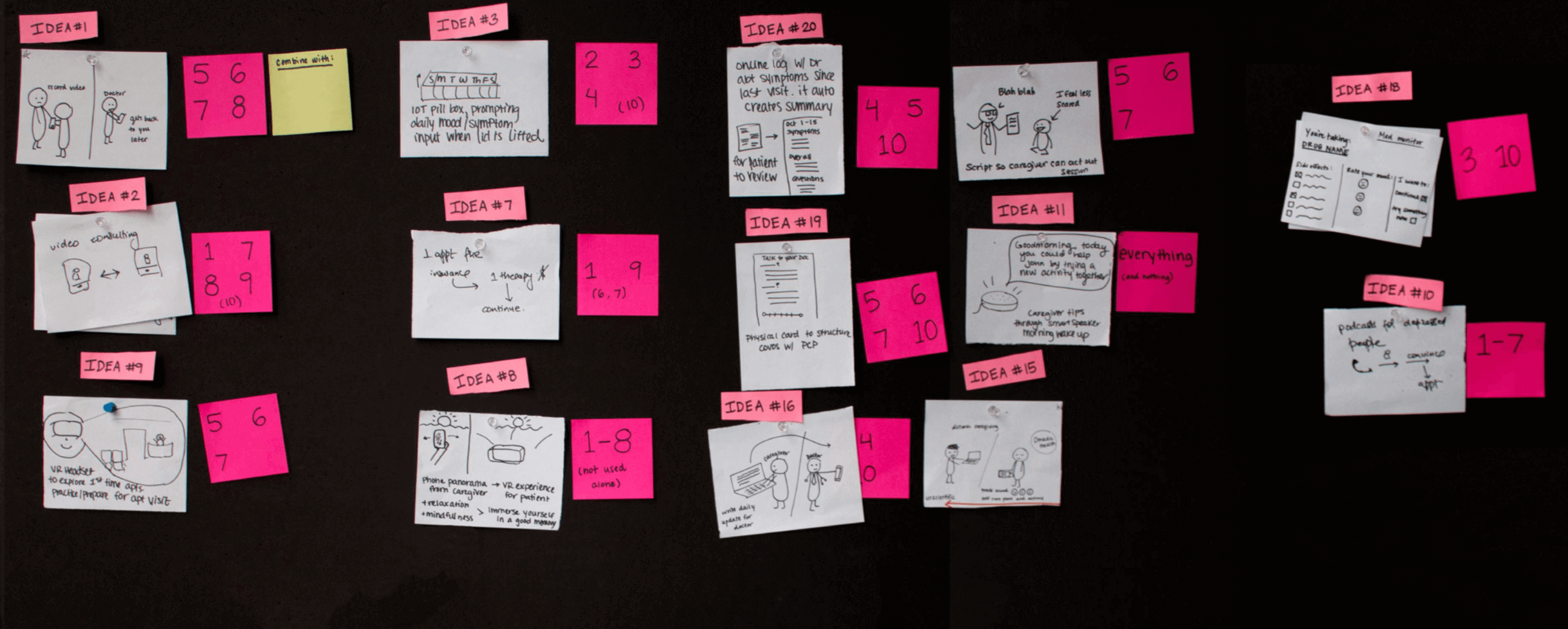
20 down-selected ideas. Along with each idea, we listed down all possible combinations which help build a stronger and cohesive product.
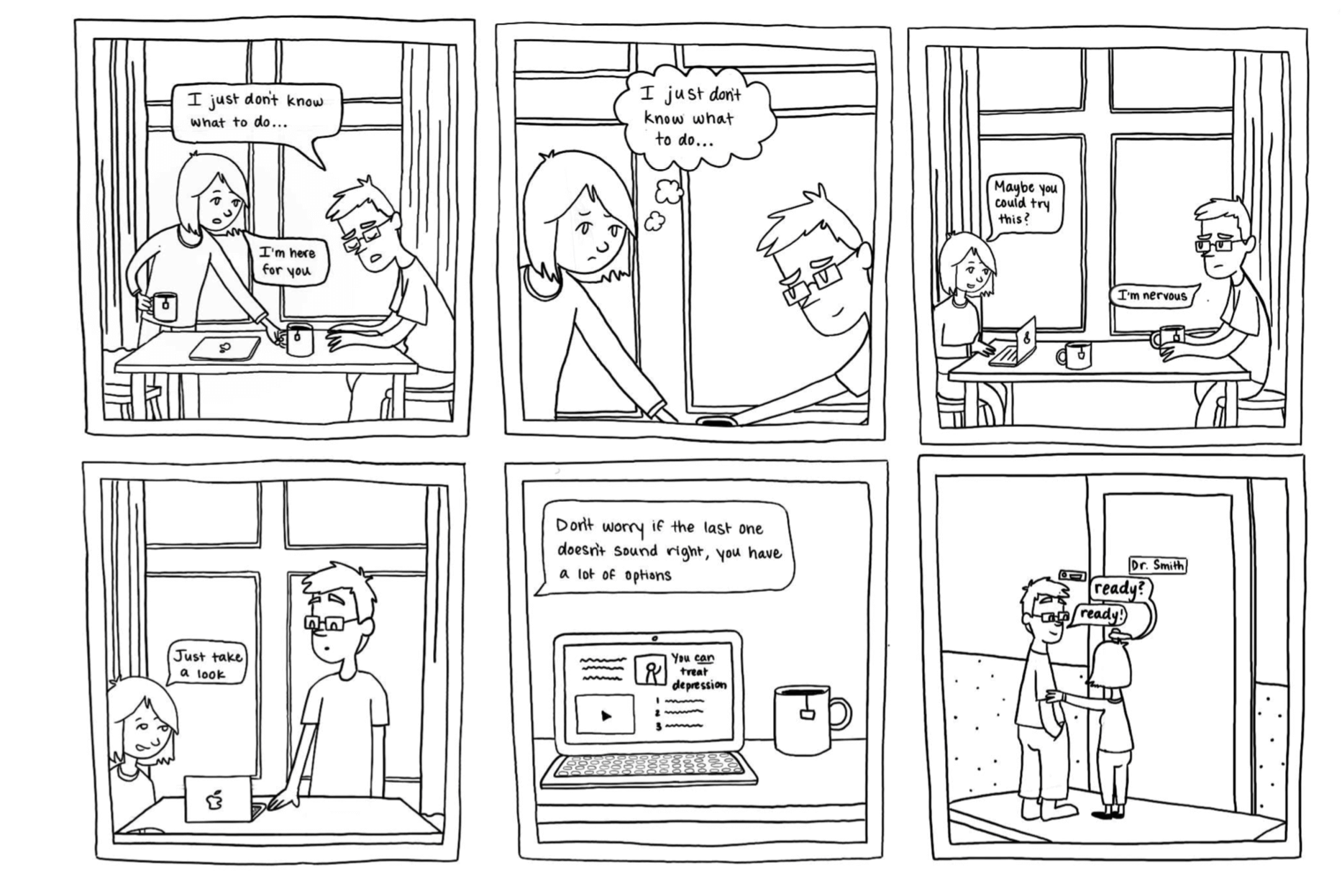
01Being There
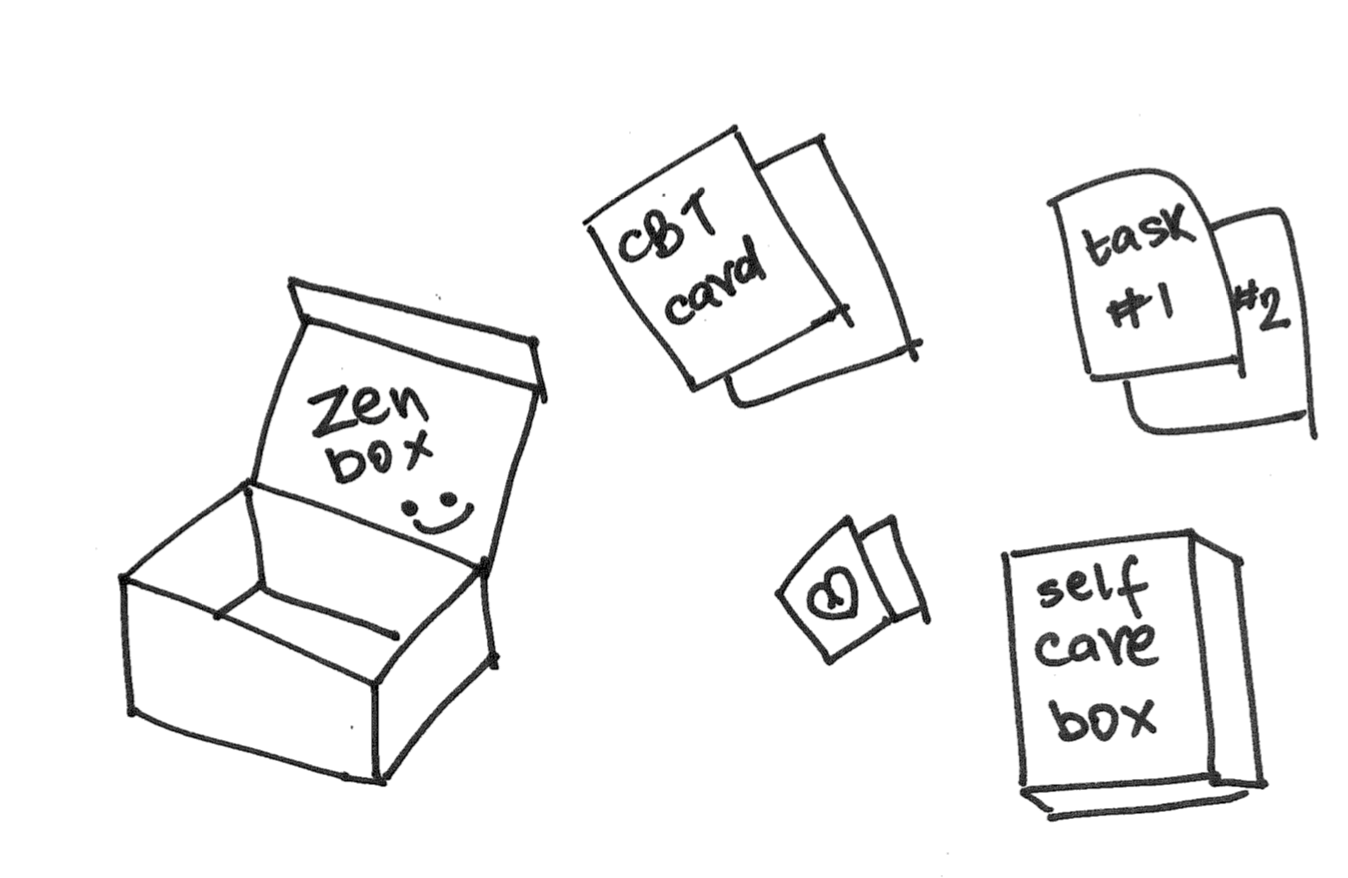
This beautiful and well crafted object aims to provide an alternate care plan to patients, to complement their ongoing medical care.
This is a physical box, designed to counter the symptoms of depression by engaging patients in alternative hobbies and tasks. It contains informational cards, alternate action cards, communication aids, caregiver calendars and emergency planning tools.
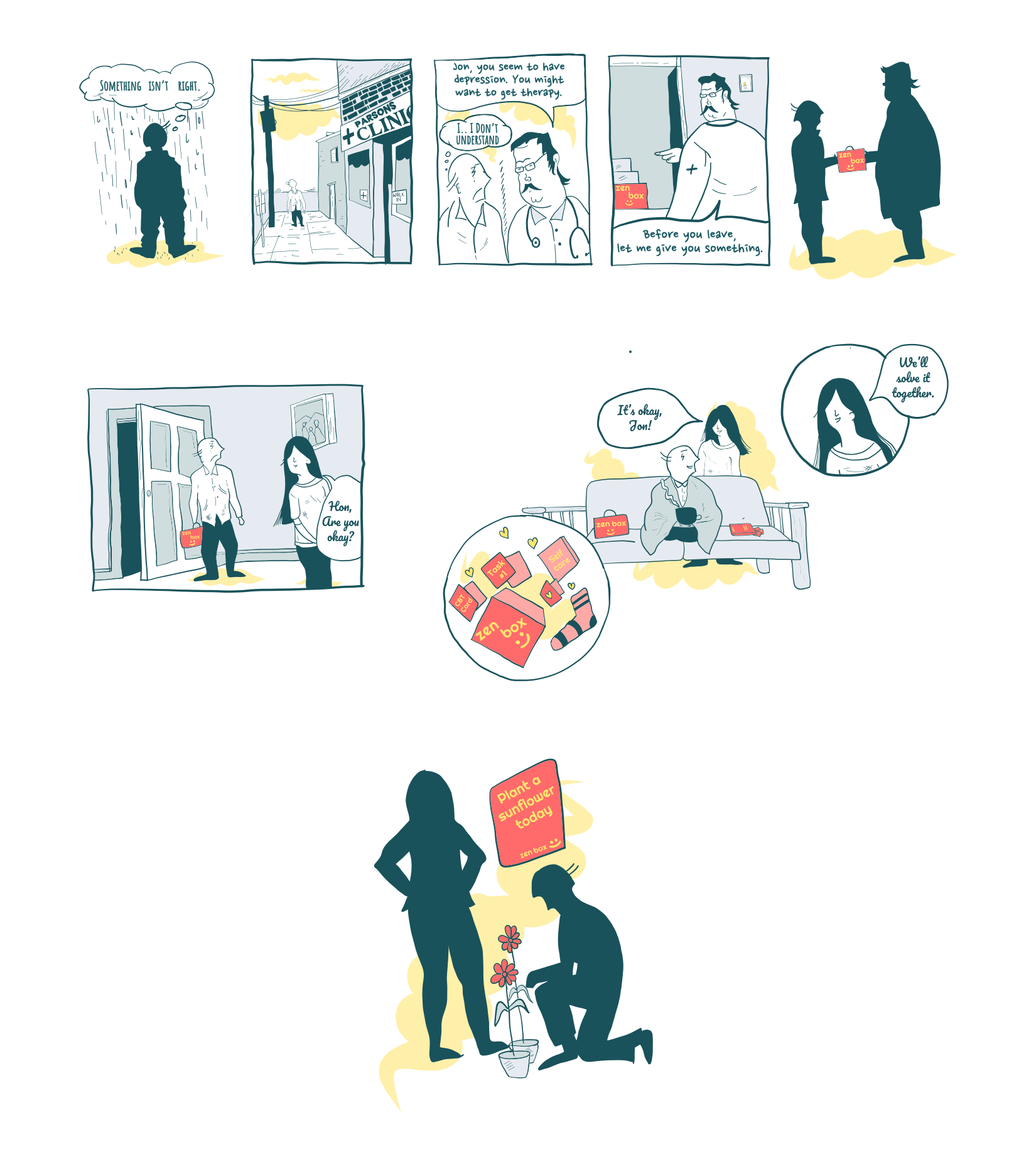
Storyboard made by me explaining the concept.
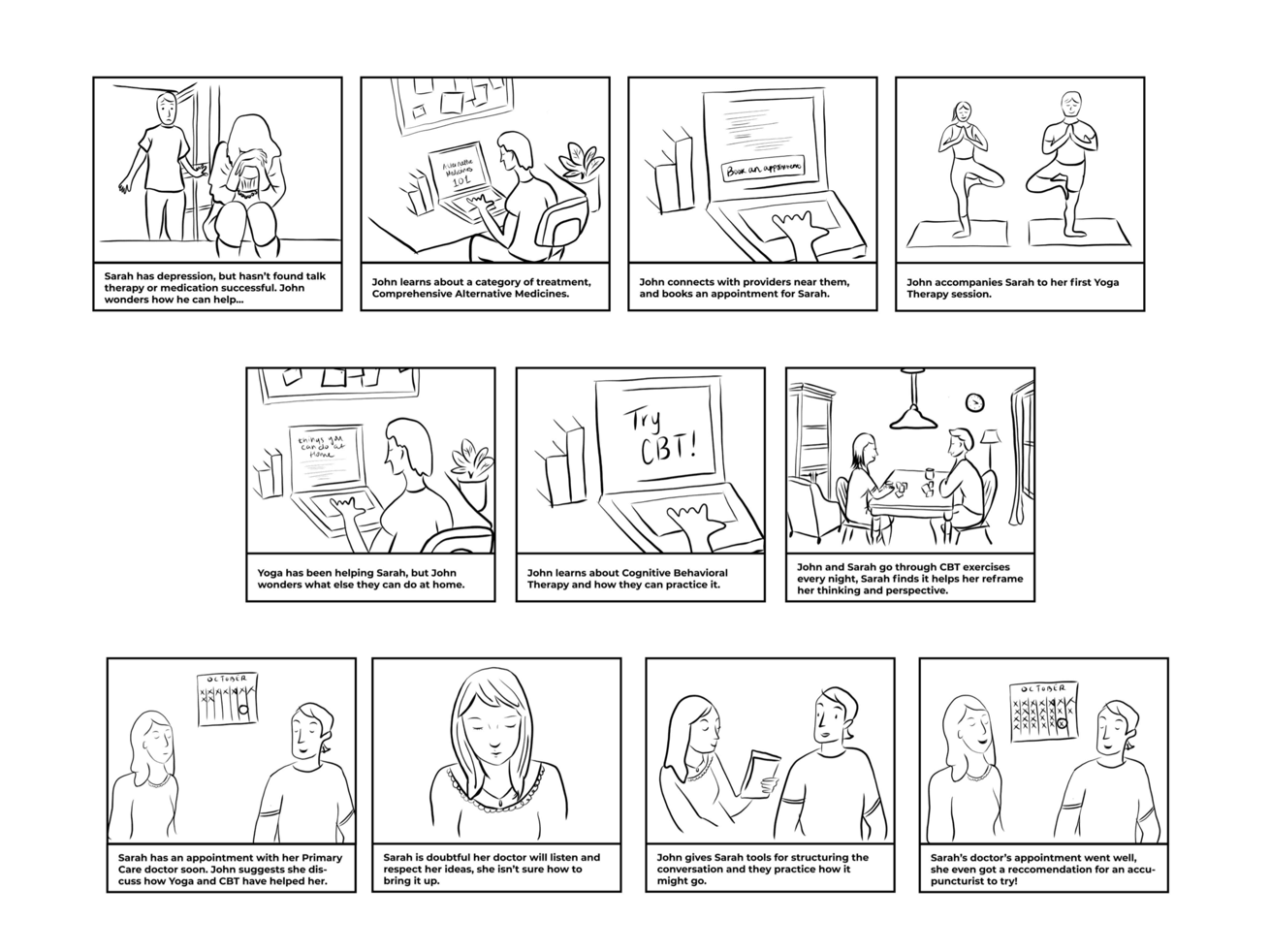
02Getting Care
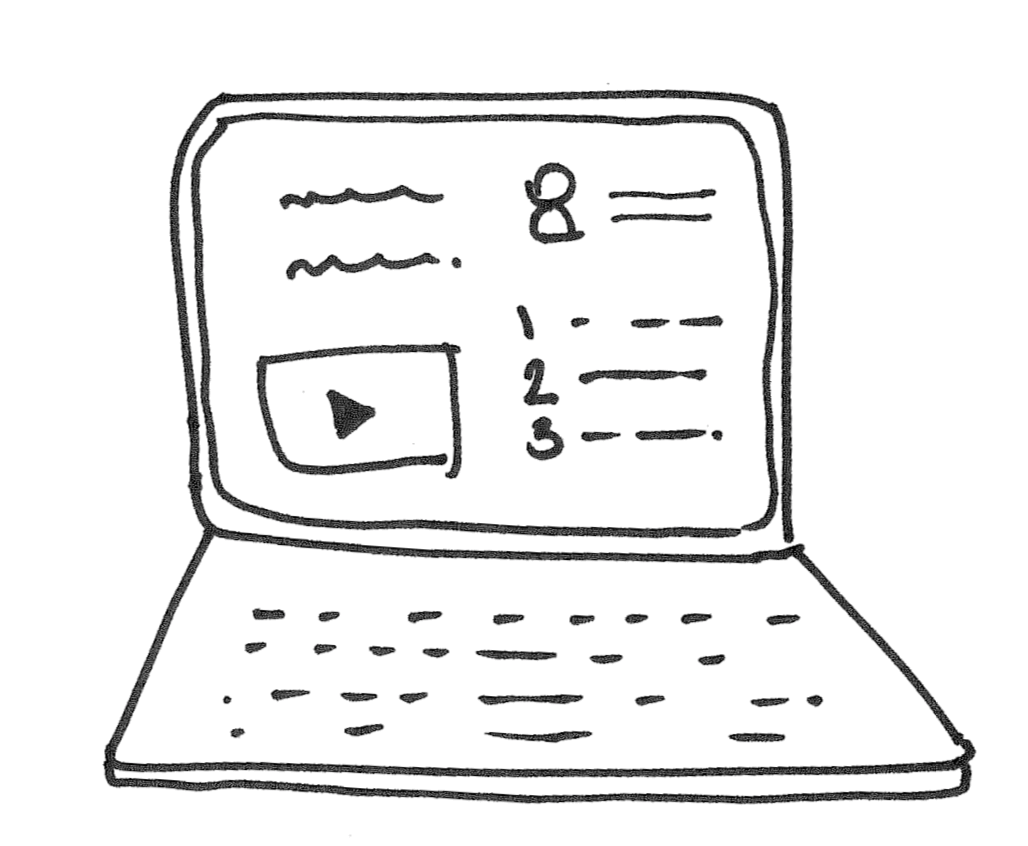
An online platform that provides information regarding what types of Comprehensive Alternative Medicine is available, connects with providers, and schedules appointments.
This is a platform for caregivers to educate themselves about their options. Contains online caregiver classes hosted by the insurance provider and transparently outlines the care options available/covered by insurance. Additionally, it also has personal success stories available for all therapies and situations.
Sam made this amazing storyboard about response 2.
03Alternative Medicine
A platform for caregivers to educate themselves about the different options for treatments, understand what they entail, and read success stories from other patients.
A set of tools for caregivers to learn comprehensively about alternative medicine options and connect with providers nearby. This also contains tools for talking about these treatment options with your primary care doctor.
This compelling storyboard, made by Nora, talks about response 3.
Prototype testing
Through user interviews and initial user-tests we realized that Response 1 stood out to be more impactful than others. However, there were elements from the other responses which could be merged together to build a more comprehensive and robust solution.
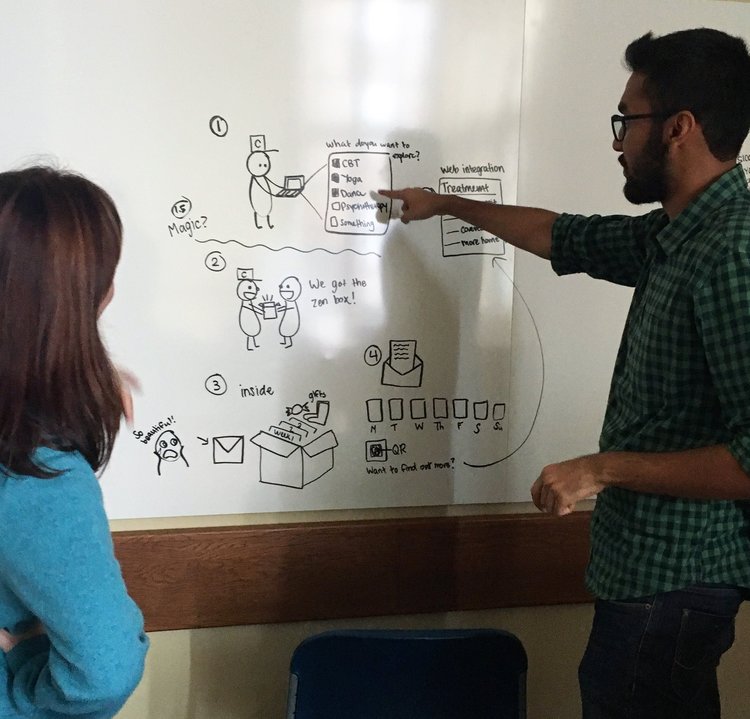
Whiteboarding the Zenbox experience map.
Hence we built Zenbox, a tool to providing caregivers with introductions to alternative care options, personalized to treat their loved one's depression.
One of the many tested paper prototypes of Zenbox
We tested the prototype with 6 potential caretakers and patients. Our aim was to test if users understood what Zenbox was, how it works, its components and more importantly what brought them joy on using it.
We received a lot of constructive feedback and learnings. The website, which serves as a marketing landing page, needs to explain the intricacies of what Zenbox is. Some also requested for helper tips and guide to have a conversation with their loved ones.
You can find more details about the results from prototype-testing below.
Read more
Defining the architecture
While testing the early wireframes of the prototype, we started framing the architecture and user-flow of the product.
The primary user's (caregiver) journey has three key paths:
- Order Zenbox online
- Try out different alternative treatment options
- Return to the website to find a practitioner
This journey is represented graphically below. Users may select up to six treatment trials, in which case key path two would be expanded accordingly.
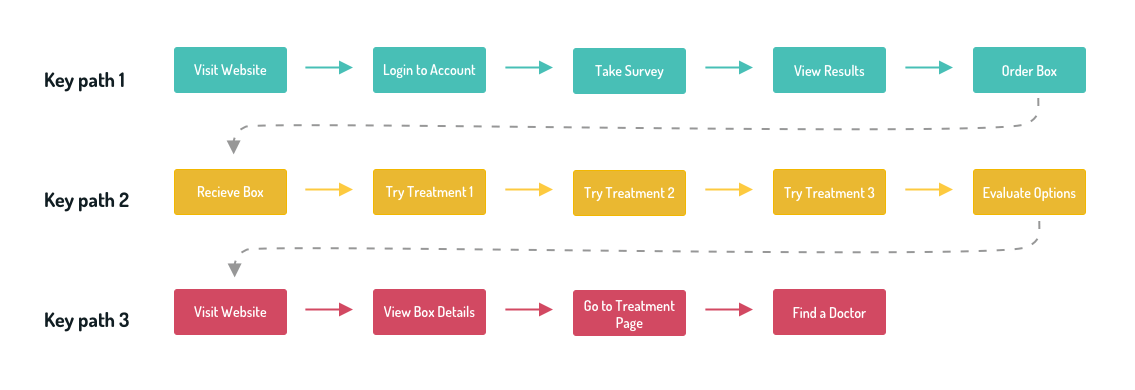
The journey of the caregiver while using Zenbox. Keypaths are explained below.
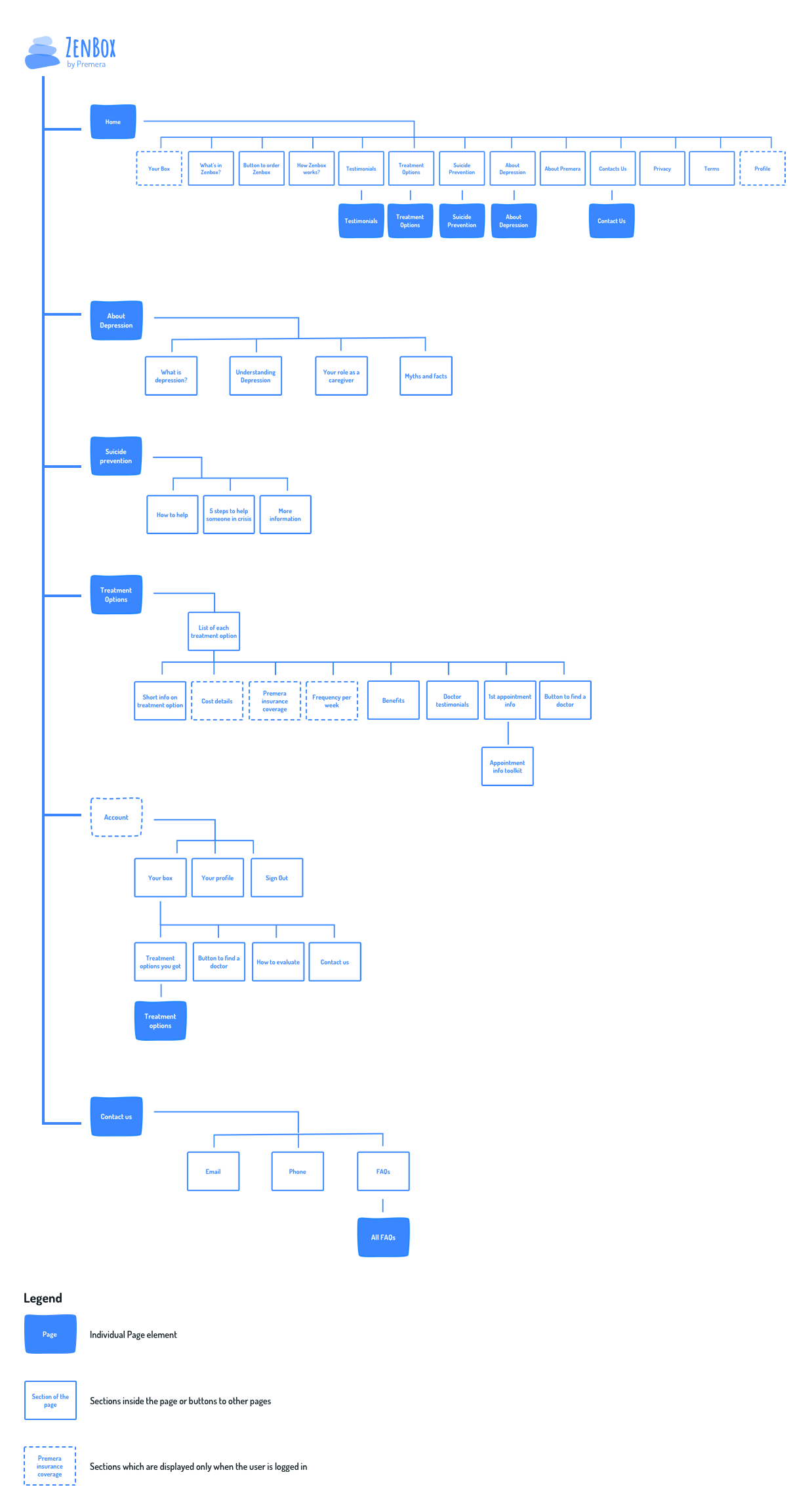
Sitemap and architecture of the companion website.
01Key path: Order Zenbox online
The landing page (Zenbox’s website) contains information about the product, detailing how it works and featuring user testimonials. The caregiver needs to provide a few details about the patient which enables Zenbox to suggest customized treatment options for the patient based on the survey.
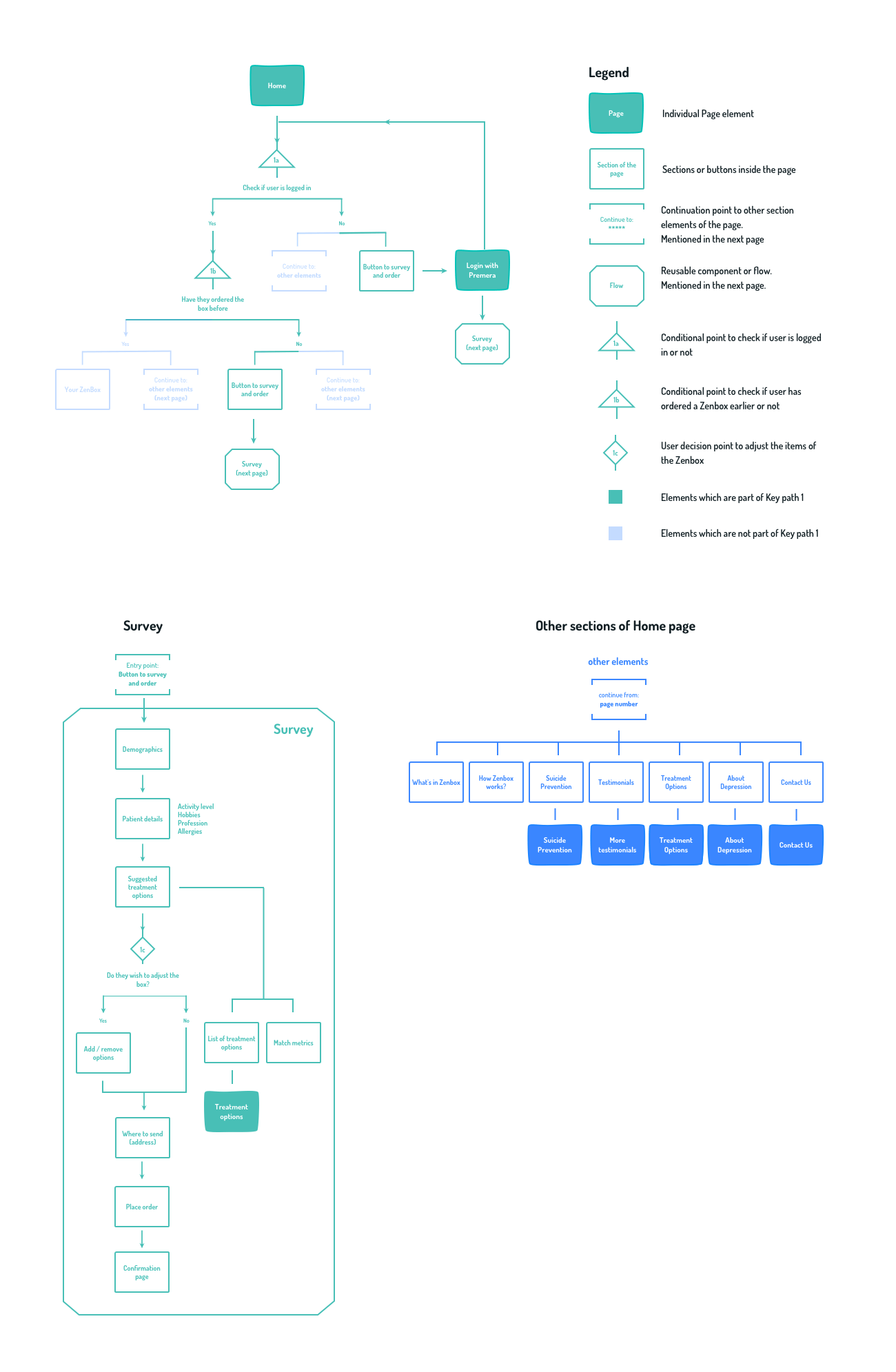
User flow for Key Path 1
Flow for caregiver to provide information about the patient.
Zenbox provides the caregiver with potential alternative options.

Physical cards from the box. These include activities (here, Art Therapy) for the patient and tips for the caregiver.
03Key path: Find a practitioner
Returning to the Zenbox website, caregivers find key information regarding their chosen course of treatment, including the average cost per month, details of insurance coverage, and the typical schedule for appointments.
Before booking an appointment they learn a bit more about what the first appointment will be like, and have the opportunity to download a support toolkit and practice with it.
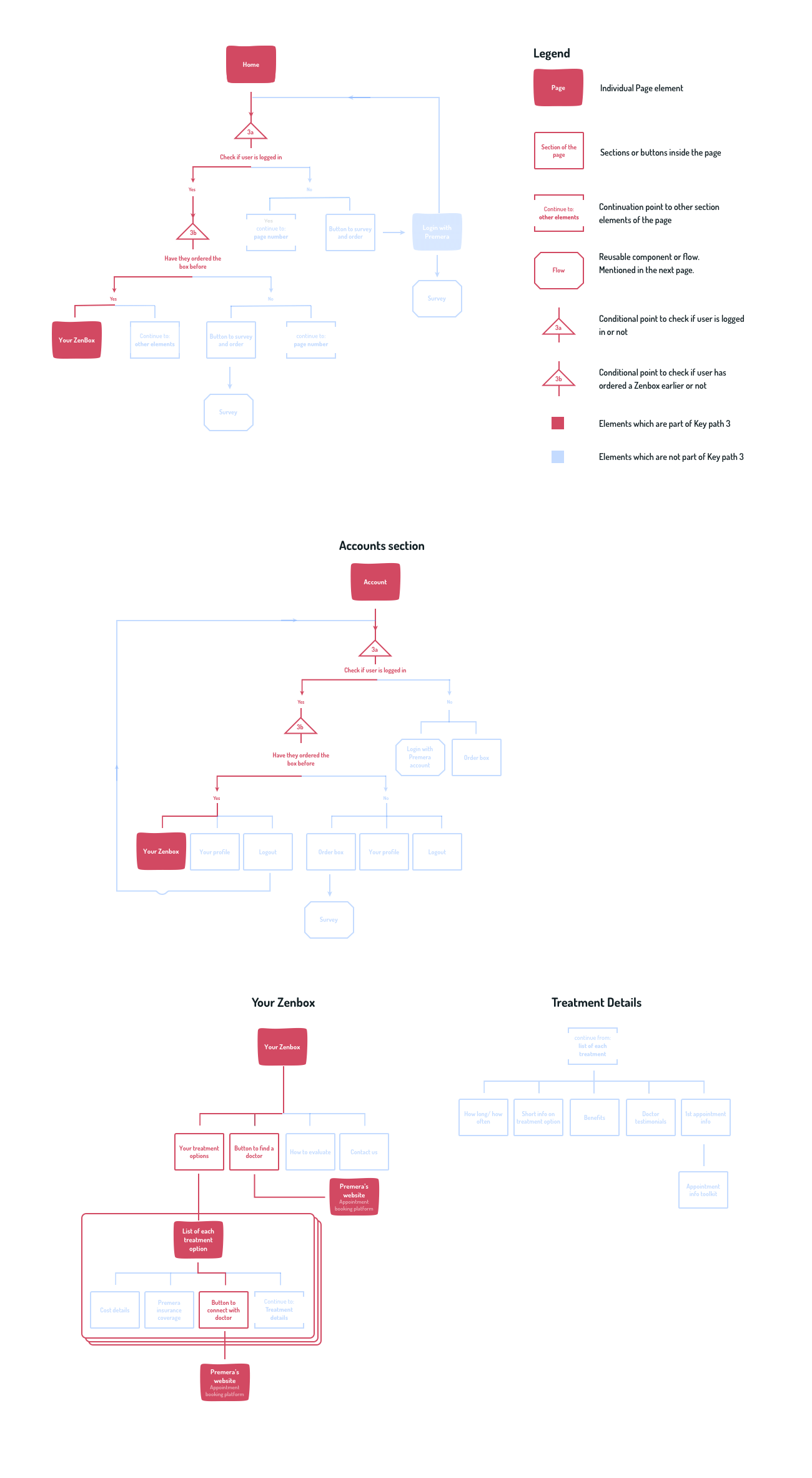
User flow for Key Path 3
Developing the UI
Our style-guide evolved during testing with users. We listened to the way they described and critiqued Zenbox, which reinforced our commitment towards a direct and personal design that puts the caregiver at the forefront.
Our primary color palette is shades of blue. Despite being blue it still has a warm feeling to it, something which echoes our design principles for Zenbox. A darker hue is used for emphasized areas.
Our secondary palette is vibrant and delightful with color applied thoughtfully and with restraint. The background shapes and illustrations use a low opacity of the color so as not to overwhelm the composition.
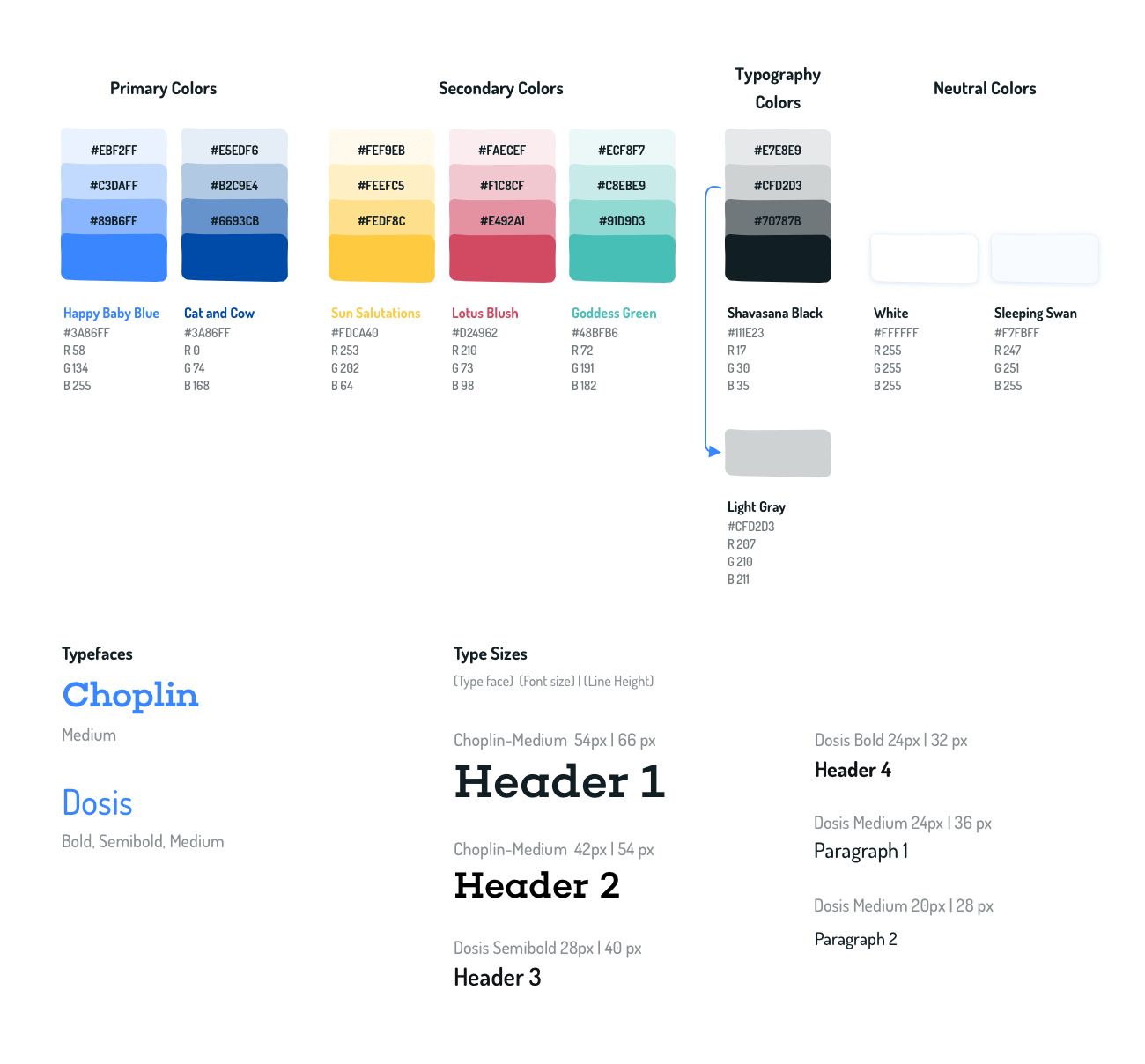
Color palette and type rules used for Zenbox
The Zenbox logo is derived from the traditions of Japanese zen rock gardens (karesensui) from around the 14th century. These gardens are meant to inspire reflection. Zenbox's stones symbolize (from largest to smallest):
- Premera (the insurance provider), who supports the ...
- Caregiver, who in turn supports the ...
- Patient with depression
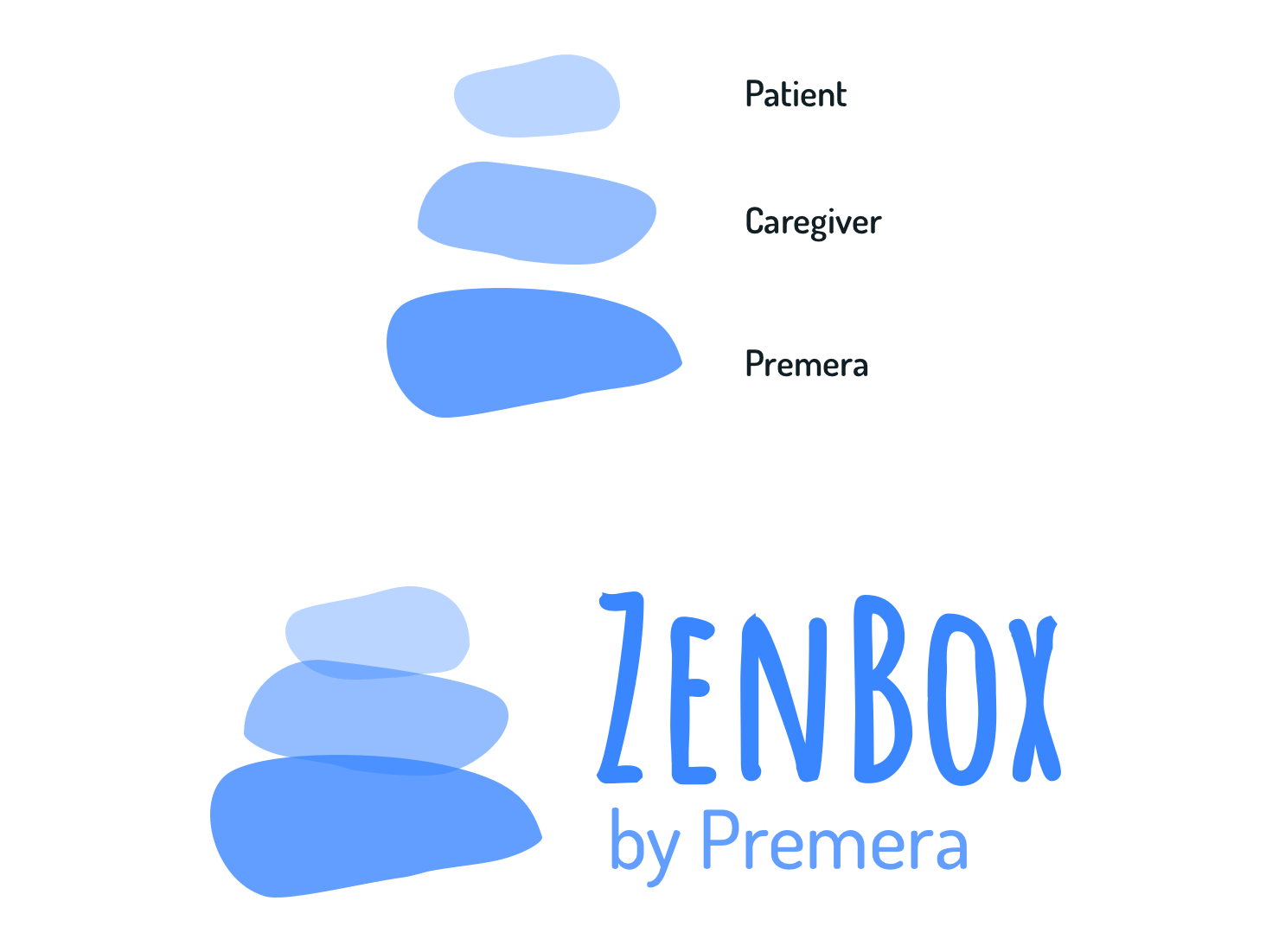
One of the possible logo variations of Zenbox
Zenbox's detailed UI specification document can be viewed through the button below.
Read more
Final design response
Our design solution caters greatly to the needs of Premera and Blue Cross Blue Shield in Washington since their patients have a higher diagnosis rate of depression as compared to the rest of the country.
At the same time, Zenbox bridges the gap between the digital and physical world, presenting informational materials in a personal and accessible way.
Zenbox website showing Key Path 1. The caregiver visits Zenbox's website and places an order for the box.
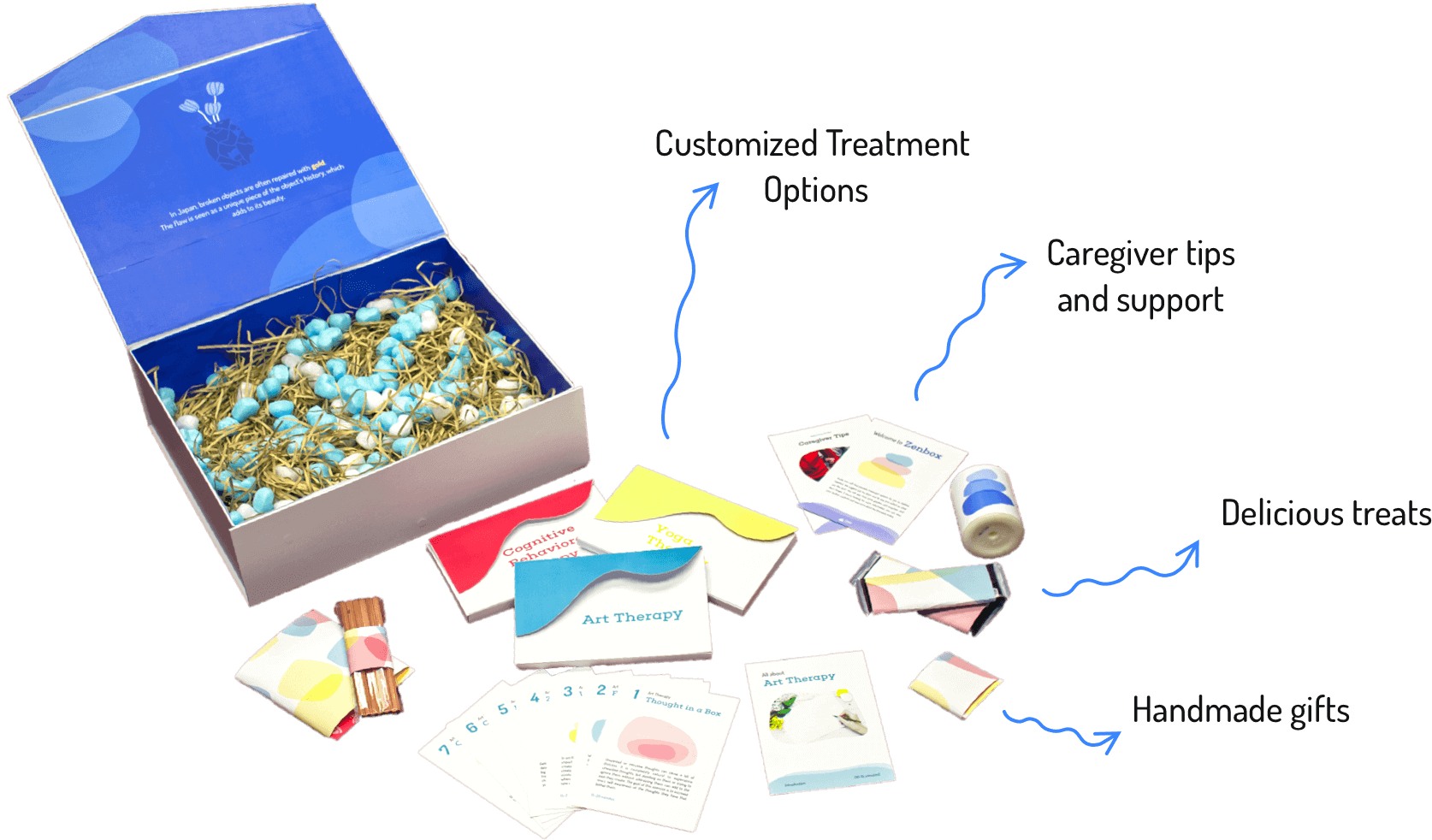
The box contained customized and personalized treatment options, caregiver tips, delicious treats and hand-crafted gifts.
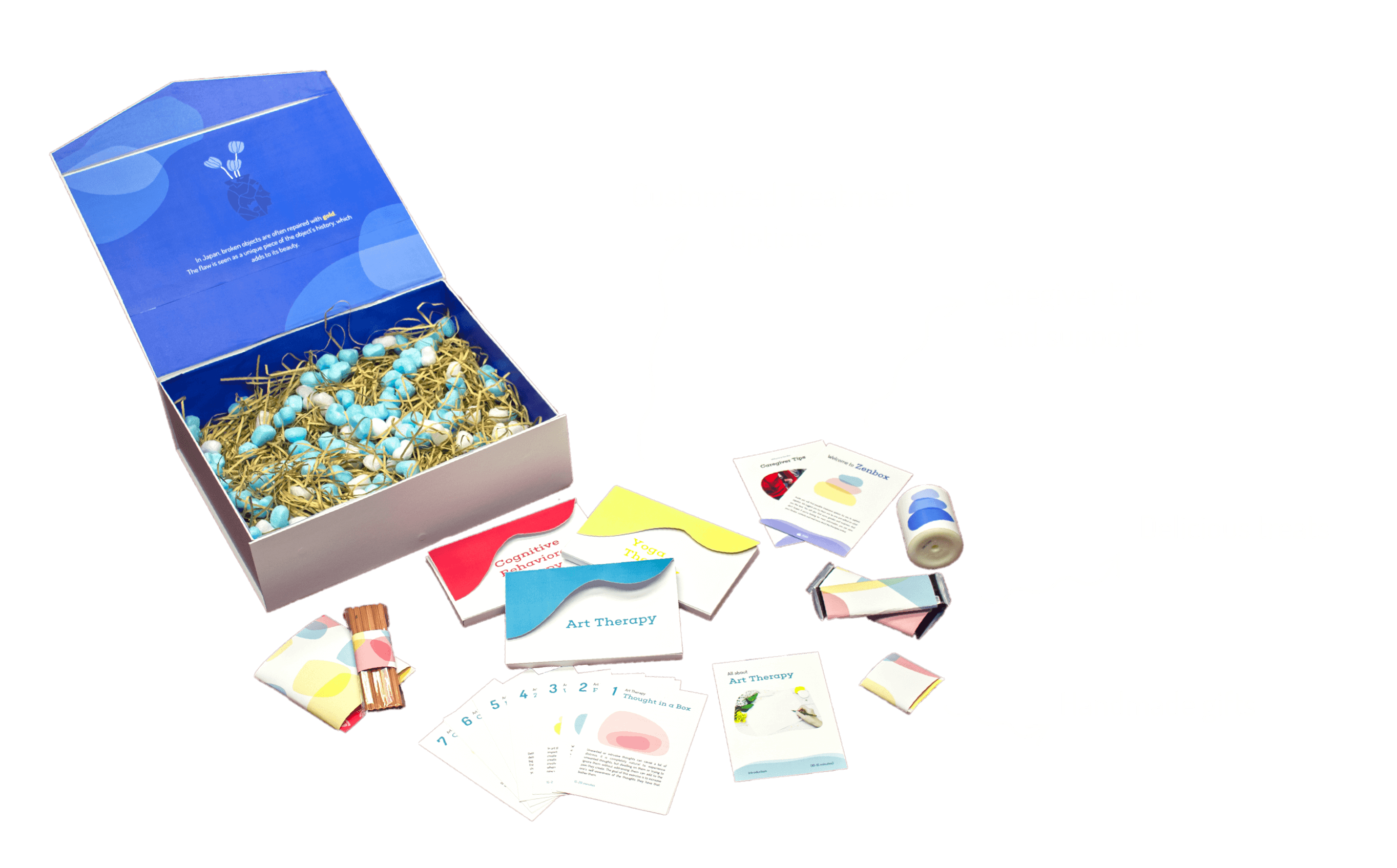
The Zenbox with 3 possible treatment plans and gifts.
The caregiver now returns to the Zenbox website to book a doctor appointment (Key Path 3).
Reflection
Our team was selected as one of three teams to present to an executive audience at Premera. The team from Premera later expressed interest in the project and are trying to build a product out of our response.
We utilized the diverse skills of our team to create a solution which we all are proud of. However, I truly believe that the idea needs to be tested and validated with medical specialists. Hopefully, Premera would be taking care of this with their highly experienced staff.
At the same time, I did not account a lot into the business viability of the response. I did some brief cost analysis and mapping those to the market oppurtunity gave positive signals. But these surely need to be validated.